Food consumption and associated risks
Hazards that may adversely affect our health are inherent in all human activities, including activities related to food production, such as capture-based aquaculture. Knowledge of the risks associated with seafood consumption is based on epidemiological data that are not always properly understood.
The identification of hazards and the determination of their relevance to health, as well as their control, are functions of risk analysis. Risk analysis is an emerging discipline in food safety, and forms the methodological basis for assessing, managing and communicating the risks associated with food-borne hazards. There is a fundamental difference between a hazard and a risk. A hazard is a biological, chemical or physical agent in food, or a condition of food, with the potential to cause harm. A risk is an estimate of probability and severity to exposed populations from the adverse health effects resulting from hazards in food. Understanding the association between the reduction
in hazards associated with food and the reduction of risk to consumers is of central importance in the development of appropriate food safety controls (Figure 146).
All foods can transmit disease, including fish, shellfish and fish products. Food-borne outbreaks are usually defined as the occurrence of two or more cases of a similar illness resulting from the ingestion of common food (Huss et al. 2000). In Europe (42 countries), fish, shellfish and fish products were identified as vectors in 5.3% (6th in importance) of the human disease outbreaks investigated in the period 1993-98 (WHO 2001). In other areas problems have been linked to the high consumption of raw fish (which creates further hazards) and of certain potentially toxic species, such as puffer fish, that are highly risky (and whose consumption is forbidden in most countries). These problems can be largely prevented and controlled through appropriate food-safety measures but a

Figure 146. Food safety controls (Source: FAO)
number of problems remain, even after the application of Good Manufacturing Practices (GMP), Good Hygienic Practices (GHP), and HACCP principles in the processing of certain types of seafood. For example, there are insufficient controls for monitoring and regulating biotoxins in fish (e.g. ciguatera).
General hazards associated with wild and farmed seafood
The traditional habit of consuming raw (uncooked) seafood in certain countries is an area where prevention of food-borne illnesses is not well developed. The true incidence of illnesses transmitted by seafood is not completely known. Few countries have established reporting systems for seafood-borne illnesses, so data is scarce. Nevertheless, available epidemiological data is useful in demonstrating trends and identifying areas of concern.
Generally, the number of cases resulting from seafood ingestion is small compared to those caused by meat products. However, the importance of seafood as a vehicle for disease depends on a number of factors, such as the diet of the population and the traditional ways of preparing food. In Japan, for example, the proportion of outbreaks due to seafood is high, since fish are an important part of the diet and a lot of fish may be eaten raw. Moreover, in Asia, the custom of eating raw fish leads to food-borne trematode (parasite) infections derived from cultured fish.
The statistics for seafood-borne illnesses show that nearly 80% of all outbreaks related to fish consumption are caused by biotoxins such as ciguatera or scombrotoxin (Huss et al. 2000). While the presence of biotoxins in fish is related to certain geographical factors (warm tropical waters), the formation of scombrotoxin (biogenic amines) takes place in specific fish species post mortem (such as Scombroidae and Clupeidae) – particularly when these fish are kept at temperatures of >5°C (histamine may also be formed at temperatures below 5°C; it depends on the type of fish flora). Only 12% of seafood-borne outbreaks are due to bacteria (Clostridium botulinum, Escherichia coli, Salmonella spp., Staphylococcus spp., Vibrio spp., Bacillus cereus). Unfortunately, the statistics do not include information on the types of fish products, which were consumed prior to the outbreaks of illness. Knowledge of the safety principles involved in fish processing, e.g. pH, smoke, additives, packaging and preparation before eating (cooked or uncooked products), is useful to evaluate the hazards related to fish products.
The hazards associated with finfish, whether wild or farmed, can be grouped into pre-harvest contamination and harvesting and processing contamination.
Pre-harvest contamination
Pre-harvest contamination mainly involves biological hazards: bacteria, parasites, biotoxins from toxic algae and, to a lesser extent, chemical hazards.
The hazards associated with human pathogenic bacteria in finfish can be divided in two groups: those naturally present in the aquatic environment (referred to as indigenous bacteria) and those present as a result of contamination with human or animal faeces or otherwise introduced into the aquatic environment (Feldhusen 2000). At least ten genera of bacterial pathogens have been implicated in seafood-borne diseases (Figure 147):
? bacteria which are normal components of the marine or estuarine environment (indigenous bacteria) such as Vibrio cholerae, V. parahaemolyticus, V. vulnificus, Listeria monocytogenes, Clostridium botulinum and Aeromonas hydrophila;
? enteric bacteria which are present due to faecal contamination (non-indigenous bacteria) such as Salmonella spp., pathogenic Escherichia coli, Shigella spp., Campylobacter spp. and Yersina enterocolitica.
Hazards are relevant or irrelevant according to the risk level at the time of consumption. Indigenous pathogenic bacteria, when present in fresh cultured products, are usually found at fairly low levels and, where these products are adequately cooked, food safety hazards are insignificant. If fish is consumed raw or is not properly cooked the risk can be significant. In Japan, for instance, there are a number of V. parahaemolyticus (fish normal flora) outbreaks due to consumption of raw fish.
A few bacteria associated with the faecal contamination of seafood continue to pose a large scale health threat; these are particularly relevant when culture systems are close to centres of human population, e.g. in Hong Kong. There are also situations where the fish culture system is far from human population and contamination with Salmonella spp. may exist. This happens in places where there is a large population of birds (e.g. near the coast); Salmonella spp is part of the normal flora of birds, and transfer through their droppings on cages, ponds, etc., cannot be ruled out.
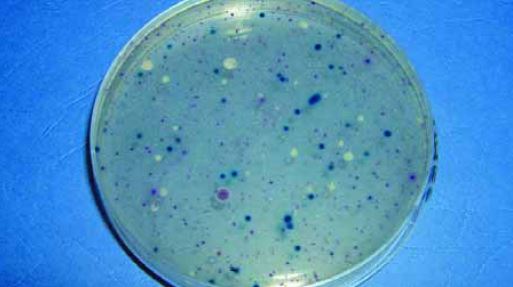
Figure 147. Bacterial seafood analysis (Photo: C. Silvestri)
Live fish may be infected with a number of pathogenic bacteria normally found in the aquatic environment, such as C. botulinum and various Vibrio spp. However, only the proliferation of these organisms can be regarded as a hazard. The severity of the diseases related to these organisms may be high (botulism, cholera) or low (Aeromonas infections), but the likelihood of provoking disease (risk) is very low. Most pathogenic strains require temperatures of more than 5°C for growth and they compete with the normal spoilage flora that proliferate comparatively more rapidly at low temperatures. Thus, products are likely to be spoiled before toxin production or the development of high numbers of pathogens. When products are cooked before consumption, and no further contamination takes place, the risk is largely reduced, as the bacteria and their toxins are heat sensitive (Feldhusen 2000).
In the last 15-20 years there has been an increasing concern worldwide about Listeria monocytogenes and its implications for food safety. It has been found in processed seafood products, such as cooked or frozen seafood, marinated fish, “surimi”, “sushi”, and smoked fish. The hazard for human health is listeriosis; in Germany there have been an estimated 200 cases per year in a population of 80 million (Feldhusen 2000). At present, there have been no reports of epidemic outbreaks due to this bacteria in the fish products consumed globally;
L. monocytogenes has been identified as the causative agent in only a few cases. However, the incidence of Listeria in fish products is very high in Latin America; in Brazil it was found in domestic and imported seafood, whether raw or ready-to-eat, but the real incidence of Listeria is difficult to assess (Destro 2000). Pre-harvest contamination with pathogens from the animal/human reservoir (Salmonella spp., E. coli) can cause illness but, again, normal cooking procedures mitigate the risk that is related to the consumption of raw fish dishes such as “sushi”.
Problems related with animal feed ingredients may exist; for example, meat and bone meal (MBM) and animal by-products have been reported to have the highest incidence of Salmonella. Chemical or physical pre-treatments substantially decrease initial Salmonella population levels in feed protein sources, and have effectively lowered population levels in poultry feed; however Salmonella may survive long-term storage (Ha et al. 1998).
The presence of parasites constitutes another biological hazard; a large number of fish species can serve as sources of parasitic infections (WHO 1995). In Japan, about five species of parasites affect humans. Among them, the most important is Anisakis simplex, which is uncommon in humans since it is killed by normal cooking or freezing of fish products but the consumption of uncooked seafood (e.g. “sushi”) can cause anisakiasis (Ogawa 1996; WHO 1999). This is especially noticeable in communities where eating raw or inadequately cooked fish is a cultural trait; about 2 000-3 000 cases are reported every year in Japan. The juvenile stage of this parasite infects humans through several cultured fish species.
The most important biological hazards are biotoxins, whose occurrence is widespread. In pre harvest contamination, ciguatera constitutes the main hazard. Ciguatera is a global problem caused by the consumption of warm-water fish infected with ciguatoxins, a family of heat-stable, lipid-soluble, highly oxygenated, cyclic polyether molecules. They have their origin in Gymnodinium toxicum, a benthic dinoflagellate that is at the base of tropical coastal marine food chains (Lewis and Holmes 1993). More than 400 species of fish can be involved in ciguatera poisoning. Ciguatera is mostly confined to the Pacific, Western Indian Ocean and the Caribbean seas; in fact it has a greater socio-economic impact in those regions where fish is the principle source of protein (Lewis 1992). The affects of ciguatera poisoning can last for several weeks or months; gastrointestinal symptoms, such as vomiting, diarrhoea, nausea and abdominal pain typically occur, often associated with neurological problems. Effective treatment of ciguatera requires accurate diagnosis, and intravenous mannitol is a possible treatment. Detecting ciguatoxins is difficult, mostly due to their low levels in ciguateric fish (<0.05 ppb for one common type of ciguatera molecule). Detecting ciguatera is even harder when different classes of these biotoxins coexist, as in Hong Kong where both Pacific and Indian Ocean ciguatoxins occur (Lewis 2000).
The potential hazards due to chemical contaminants in fish and fish products from aquaculture include heavy metals, dioxins, dioxin-like PCBs and similar substances, and residues and unauthorized substances. Heavy metals, such as mercury, cadmium and lead can be tolerated by humans only at extremely low levels. Fish can accumulate substantial concentrations with respect to mercury in their tissues and thus represent a major dietary source of this element. Fish are known to be the largest mercury source, with the exception of direct exposure. The use of chemicals in fish culture is regulated in the USA and in Europe; in some countries regulations may exist but most have no regulatory body to control their use.
Dioxins are mainly a man-made hazard, resulting chiefly from the incomplete combustion of urban wastes. The term “dioxins” is a generic name that encompasses two different types of compounds, the polychlorinated dibenzo-p-dioxin (PCDD) (75 congeners) and the polychlorinated dibenzofurans (PCDF) (135 congeners). Seventeen of these compounds are of recognized toxicological human concern.
Polychlorinated biphenyls (PCBs), also known as “dioxin-like”, are a family of 209 congeners, of which about thirteen are of toxicological human concern. PCBs are also a man-made hazard; they were mainly produced for industrial use in electrical equipment (transformers and capacitors). The international treaty on persistent organic pollutants (POPs), drafted by 122 nations in South Africa in December 2000, targeted PCBs as one of the dirty chemicals to be phased out globally. Some countries, in particular developed countries, banned the production of PCBs many years ago (e.g. the USA in 1976). However, due to the persistence of PCBs in the environment, they continue to be a food hazard, even in countries that banned their production a long time ago.
Dioxins are only slightly volatile, and therefore tend to show limited geographical distribution (e.g. a lake, or a portion of a river) mainly following fallout from the smoke plumes of combustion, and in water courses thereafter. By now, however, they can be found in many areas all around the world. PCBs have low water solubility (also they remain on the water surface). However, in contrast to dioxins, PCBs are highly volatile; the result is that PCB contamination can be found worldwide, including the Arctic and Antarctic regions. Both dioxins and PCBs are highly soluble in lipids and therefore tend to accumulate in animal and human lipids. Fat in milk, meat, eggs, fish and their products are the main source of dioxins and PCBs in our diet.
Dioxins and dioxin-like compounds may be accumulated in fish, either from the water with which they are in contact (freshwater or seawater) or from contaminated feeds. In practice it is impossible to avoid some contamination with dioxins and, in particular, PCBs; however, it should be possible to avoid specific geographical locations (land or water) that may be exposed to significant contamination by dioxins and PCBs. Accumulation of dioxins and PCBs by fish directly from water is possible, but this route is generally considered negligible for species at the top of the trophic chain.
Usually, high-energy feeds are the first cause of concern. Studies conducted in various countries have shown that cultured fish, particularly those reared on aquafeeds containing fishmeal and fish oil, exhibit levels of dioxins and dioxin-like substances greater than those found in wild fish (Easton, Luszniak and Von der Geest 2002; Hites et al. 2004). These findings could also be related to the amount of these substances in the fish feed used, particularly in the fishmeal and fish oil incorporated. Limits for dioxin and dioxin-like substances in fish and fish products exist in almost all countries (for example, in the case of the European Union, Council Regulation (EC) No. 2375/2001, 29 November 2001, applies). Despite the findings mentioned above, it is important to note that all studies to date have shown that the levels of dioxins and PCBs in both wild and farmed fish are generally well below regulatory and advisory limits; however, concerns about this type of hazard remain.
Regular surveillance, particularly in developed countries, shows that levels of dioxins and PCBs in the human diet and in body lipids (e.g. mothers’ milk and blood) have generally fallen substantially since the mid-1980s, following the enforcement of improved regulations on garbage combustion, the ban on the production of PCBs, and the development of regulations regarding the disposal and handling of PCBs. Nevertheless, the risk of these types of hazards may be significant in specific geographical areas where such measures do not apply, or only partially apply, or due to the faulty implementation of regulations.
Other possible sources of chemical contamination may include fertilizers, pesticides, drug residues, disinfectants, chemotherapeutants, medicines for disease control in fish, antifoulants used in cage nets, etc. The number of possible hazardous substances is very large; therefore specific hazard analysis may be necessary in each specific location. In any case most countries have regulations that define the specific obligation to establish an approved residue-monitoring plan for aquaculture that includes fish, water and sometimes feeds.
The potential exists for the strains of some human pathogens, such as Streptococcus (Weinstein 1997), to develop high antibiotic resistance, resulting in infections that can be more difficult to treat. Resistance can spread to other types of bacteria and human pathogens, through gene transfer mechanisms special to bacteria (Dixon 2000).
Preventing pre-harvest contamination is quite difficult, since most of the pathogens occur naturally but can be controlled by Best Management Practices. If operators are to remain competitive, they will have to follow the market pressure to achieve improved Food Safety Standards and bear the high economic cost of prevention procedures.
Risks of contamination in harvesting and processing
The way in which fish are harvested may also impact quality. It follows therefore that good techniques are very important to reduce the risks of contamination. The stress due to the transportation and handling of live fish during the rearing process and during partial harvesting can also cause an immunodeficiency, decreasing their resistance to infections by pathogens, bacteria, etc. Oxidative stress research is particularly important in the health assessment of farmed fish; stressed fish are more vulnerable to disease due to an impairment of their antioxidant defence systems (Ferrante et al. 2003).
During the harvesting and processing of the various fish products, pathogenic agents that are present in the raw fish may survive in the final product. Further contamination may also occur, due to biological (bacteria, scombrotoxins, parasites) and physical hazards. Human pathogens that may contaminate the fish product during post-harvest handling include Bacillus cereus, Listeria monocytogenes, Staphylococcus aureus and Clostridium perfringens (Feldhusen 2000). Clostridium botulinum is an ubiquitous, spore-forming, anaerobic organism that produces a neurotoxin causing life-threatening food-borne illness. C. botulinum type E is naturally found in aquatic environments and is often isolated from fish. The mere presence of Clostridium botulinum in or on a fish product will not cause illness, however; viable C. botulinum spores must also be given the opportunity to germinate and produce toxin. If the fish are properly handled and processed, to prevent growth of the organism and production of the toxin, there should be no risk of botulism. Although the hazard of C. botulinum toxin is serious, the risk is low because of the implementation of strict specific regulations (e.g. LACF – Low Acid Canned Food) in many countries. Another form of toxins are the scombrotoxins, which will be described in a later section because of their particular importance in capture-based aquaculture.
The allergy producing substance histamine will develop in fish where large amounts of free histidine and bacteria are present. Histidine may be converted to histamine if the products are stored at elevated temperatures for a sufficient time. The dynamics of histamine formation depend on a number of factors, for instance the type of fish flora, the ratio between external surface and weight, high temperature/shorter time and inappropriate handling of the fish. The higher temperature allows the bacteria that decarboxylate histidine to histamine to proliferate and produce substantial amounts of the active agent, the enzyme histidine decarboxylase (Chamberlain 2000). High histamine levels indicate that the fish have been stressed during the harvest operation and stored at high temperatures for a prolonged period, giving rise to toxicity. Sedation of the fish during harvesting, and effective temperature controls during handling and processing, are practical solutions to minimize this hazard. In the past, high histamine levels in seafood products exported from the Indo-Pacific region have resulted in severe economic losses and a number of importing countries have now introduced regulations on the maximum allowable histamine content (Chamberlain 2000). For example, the United States Food and Drug Administration has established an upper histamine limit in raw and frozen tuna of 50 ppm, and has also specified a health hazard (scombrotoxic) limit of 500 ppm (USFDA 1996). Histamine is considered a toxic or deleterious substance because, if ingested at sufficiently high levels, it is known to cause scombroid poisoning. The presence of other amine decomposition products in fish may also have a synergistic effect of histamine toxicity (Lehane and Olley 2000). Histamine fish poisoning (HFP) is a mild illness, but it is important in relation to food safety and international trade. HFP occurs throughout the world (Mines, Stahmer and Shepherd 1997); however, there are no reliable statistics on its incidence. Since 1970, the countries with the highest number of reported cases are Japan, the United States and the UK. Fish containing histamine may look fresh in terms of appearance and colour; therefore such quality attributes are not adequate to assess the presence or absence of histamine. HFP is a significant public health and safety concern; it was first diagnosed in 1828, and since then it has been described in many countries, being now the most prevalent form of seafood-borne infection in the United States.
Consumers are becoming more demanding, and litigation following food poisoning incidents is more common. Producers, distributors and restaurants are increasingly held liable for the quality of the products they handle and sell. Such forms of illness, which are a consequence of improper handling or storage of fish, need to be controlled by effective testing methods to identify those fish likely to be toxic. Control and prevention are possible (Lehane and Olley 2000), and many countries have set guidelines for maximum permitted levels of histamine in fish, following the USFDA. However, histamine concentrations in a spoiled fish are extremely variable, as is the threshold toxic dose. Biotoxins usually survive in cooked fish, while parasites are killed when fish is frozen or cooked.
The main problem associated with distribution of seafood products is time-temperature and inappropriate handling (Figure 148). Most bacteria cannot proliferate at temperatures below 5°C; thus the proper cooling of seafood during transportation becomes an important consideration. Chilled products should be loaded when the core body temperature is below 4°C for fresh products, and below -18°C for frozen products.
Few pathogens are generally present in smoked products but there is still a high incidence of Listeria. The risk posed by the consumption of cooked (fresh or frozen) fish is also low. The principal food safety risks associated with cooked products are caused by heat stable chemicals or biotoxins (ciguatera or fish containing an excess of histamines). An indirect hazard for human health is an allergic reaction to the ingestion of dead parasites; in general this risk is considered by authorities to be very low but current regulations exist, particularly in developed countries. Processed seafood sometimes also exhibit physical hazards, such as contamination with foreign material (glass, metal) (Huss, Reilly and Ben Embarek 2000). Maintaining healthy conditions during processing can be achieved through preventative measures, such as GMP, effective hygiene and sanitation programmes, etc.

Figure 148. One of the major problems in seafood distribution is inappropriate handling (Photo: M. Nakada)